I was disappointed not to get called today in the Parky Charter debate in response to e-petition 713714. Below is (1) details about the Parky Charter and (2) the speech I would have gave in support of the charter – many thanks to Stephen Brannan (Edinburgh Parkinson’s Chair) and Clare for helping me to prepare the text.
Info on the Parky Charter – The Parky Charter is a campaign launched by the Movers and Shakers group, supported by Parkinson’s UK, Cure Parkinson’s, and Spotlight YOPD, to improve care for people living with Parkinson’s. It outlines five key demands for the UK government: faster access to specialists, immediate provision of information at diagnosis, a “Parkinson’s Passport” for automatic benefits, comprehensive personalized care plans, and increased funding for research toward a cure.
The charter emerged from widespread frustration over systemic failings in Parkinson’s care and aims to ensure dignity, timely treatment, and better support for patients and carers. Over 113,000 people signed its petition.
The Movers and Shakers group is a collective of six well-known public figures in the UK who all live with Parkinson’s disease. They originally began meeting in a Notting Hill pub to share experiences and support each other, which evolved into the popular Movers and Shakers podcast. The members include:
Gillian Lacey-Solymar – broadcaster and academic
Jeremy Paxman – former Newsnight presenter
Mark Mardell – former BBC journalist
Rory Cellan-Jones – former BBC technology correspondent
Paul Mayhew-Archer – comedy writer (The Vicar of Dibley)
Sir Nicholas Mostyn – retired High Court judge
Parkinson’s Draft Speech
Parkinson’s is the fastest-growing degenerative neurological condition in the world, but there is still no cure. In Scotland, alone, around 14,000 people currently live with the condition and, every single day, seven more Scot’s will find out that they have Parkinson’s.
Within my own constituency, Parkinson’s UK estimates there are approximately 217 people living with Parkinson’s, and across the whole of NHS Lothian this figure rises to just shy of 1800 people.
If you don’t know somebody who has been affected by Parkinson’s, you probably will soon.
Yet public understanding of Parkinson’s remains dangerously limited. Too often it is seen simply as a condition of old age or reduced to its visible symptoms: tremors, stiffness, or a shuffling gait. But Parkinson’s is far more complex than that. Up to forty invisible non-motor symptoms can profoundly affect daily life, impacting speech and swallowing, and causing bowel and bladder issues, mild cognitive impairment, dementia, and even depression.
Medication must be carefully tailored to each individual, and it often comes with unwelcome side effects. Unfortunately, its effectiveness also typically wears off over time meaning that living with both treated and untreated Parkinson’s is extremely difficult.
At the same time, our NHS – despite the extraordinary dedication of its staff – simply does not have the specialist workforce needed to support people properly: neurologists, Parkinson’s specialist nurses, physiotherapists, occupational therapists, and speech and language therapists are all in short supply. The consequence is that too many people with Parkinson’s feel isolated and unsupported while dealing with a complex, progressive disease.
When someone is told they have Parkinson’s, the question that immediately follows is: What does the future hold for me, for my family, and for those I love? Much of that emotional impact depends on how the diagnosis is delivered and while many neurologists show compassion, I am also aware of people who have received their diagnosis through the mail. Currently, provision of psychological support alongside a diagnosis is seen as optional but, if we all take a moment to imagine how receiving that letter must I have felt, I think it should be considered as essential.
As I previously mentioned, Parkinson’s is often lazily treated as a consequence of aging; however, while most people who receive a diagnosis will be over the age of 65, thousands of people of working age are also affected.
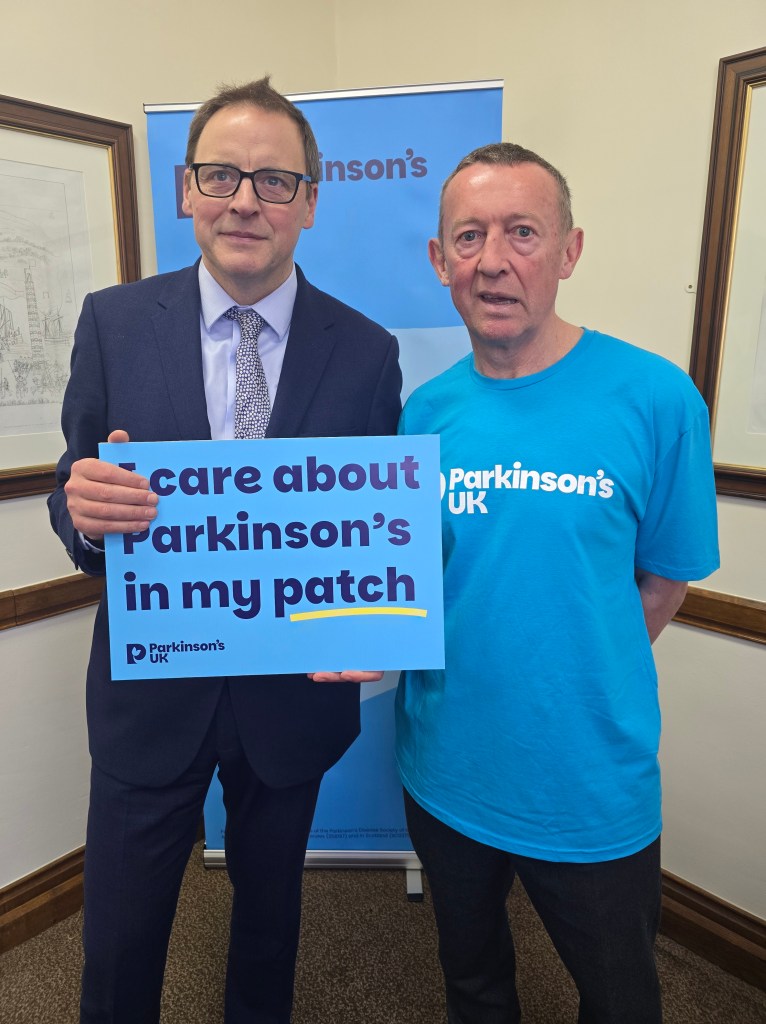
One of those people is my constituent, Clare, who was diagnosed at the age of 52. Before receiving her diagnosis she spent over £3,000 of her own money on tests and treatment and, post diagnosis, she feels she needs to continue working full-time, so that she can afford a decent level of care once she is unable to work. All of this has taken a serious toll on her health, with extreme fatigue making it difficult for her to maintain the exercise routine that we know is crucial in slowing the progression of the disease.
People like Clare show extraordinary resilience every day; the least we can do is ensure our systems – medical, psychological, and financial – match that resilience with proper investment, timely support, and compassionate care. Access to financial support, in particular, would allow Clare to reduce her hours, prioritise her health, and, hopefully, slow the progression of her condition. Her experience is not unusual, but it should be unacceptable.
